An early and accurate diagnosis is important
Perhaps you have had a strange pain that will not go away, a visible lump under your skin, or a growing discomfort after a pregnancy.1-3 These are among the many possibilities that could start the process of getting diagnosed with a desmoid tumor. A doctor could even find a desmoid tumor while looking at a completely unrelated issue.3,4
Because desmoid tumors are so rare and can appear differently from person to person, people do not always get properly diagnosed right away. In fact, desmoid tumors are misdiagnosed approximately 30% to 40% of the time.5 One of the most common misdiagnoses is lipoma.6 A desmoid tumor may also be incorrectly identified as scar tissue or another type of tumor.6,7
That can mean delays for some people in getting the care they need. But be encouraged that there are several ways to help get a timely and accurate diagnosis.
Desmoid tumors
are misdiagnosed
~30%
to
40%
of the time5
There are several ways to help get a timely and accurate diagnosis
NCCN Guidelines for Patients® provides a roadmap to help patients understand their diagnosis and treatment options. The guidelines recommend a biopsy of the desmoid tumor be performed to confirm the diagnosis. Imaging tests such as CT scan or MRI may also be needed for an accurate diagnosis.9
An incorrect diagnosis can result in delayed or incorrect treatment. This may lead to unnecessary surgery and risk of complications. Your doctor may choose to perform additional tests as well. If you have questions about getting diagnosed, be sure to ask your care team.
Evaluation and Diagnosis

Medical history and physical exam

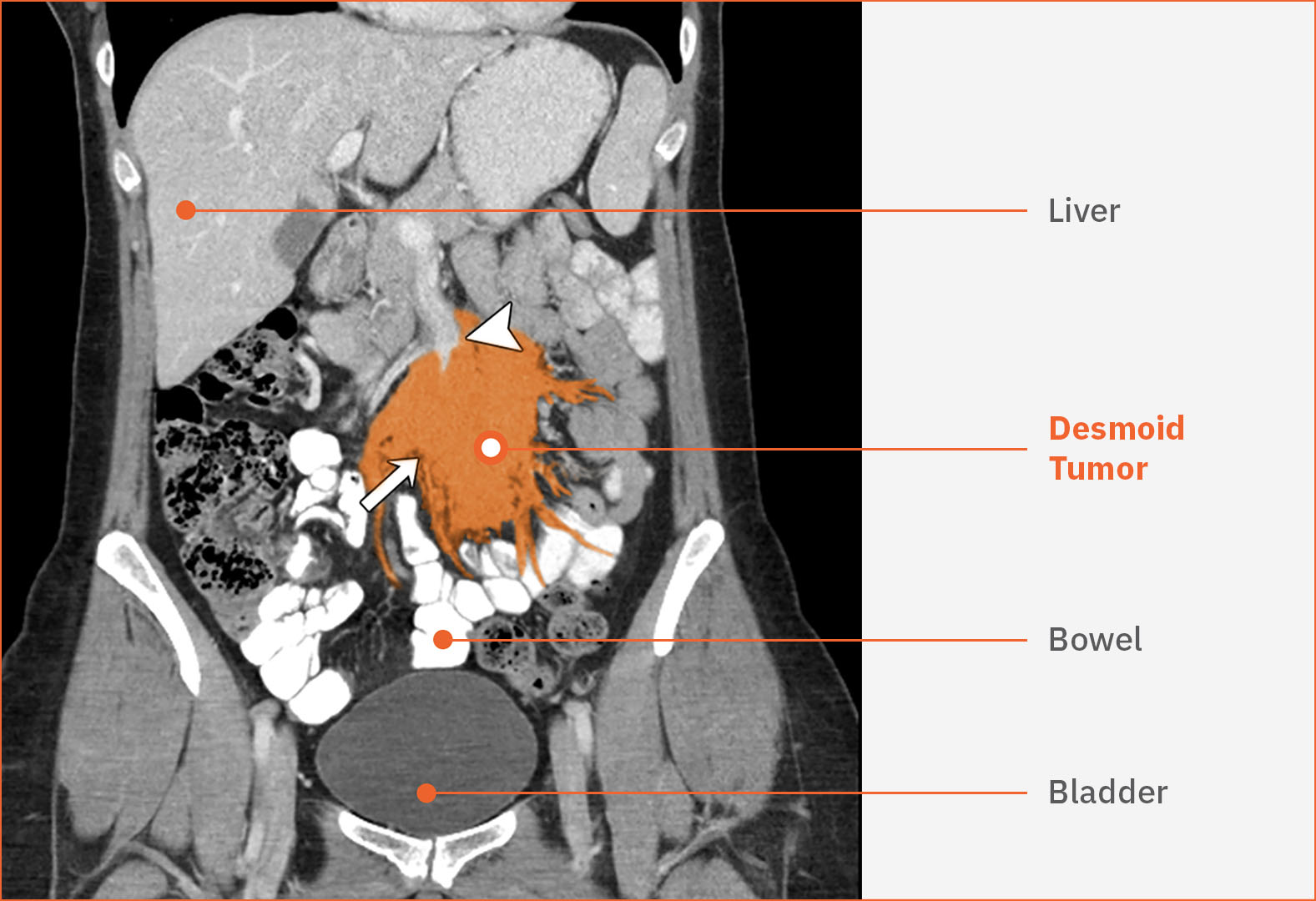
A CT scan and/or MRI10 to see what’s happening in the body can help doctors understand where the tumor is.4,11 A radiologist will review the images and write a report. They will send this report to your doctor, who will review these results with you9
Click to view scan
Intra-abdominal desmoid tumor12
This scan shows the desmoid tumor, in the center indicated by a white arrow. The desmoid tumor is surrounding a large blood vessel (white arrowhead). The tumor’s multiple tendrils are extending and threatening the bowel.

Biopsy, or a tissue sample, is needed to diagnose a desmoid tumor. A biopsy is recommended before starting treatment.10,11 A pathologist will examine this tissue sample and write a report. They will send this report to your doctor, who will review these results with you

Additional tests that may be helpful:
- Staining for beta-catenin on biopsy tissue to help doctors diagnose desmoid tumors11 Read more about beta-catenin
- Genetic testing may be recommended by your doctor to check for Familial Adenomatous Polyposis (FAP), a hereditary syndrome associated with desmoid tumors. A genetic counselor may then discuss the test results with you9
Beta catenin can play a key role in desmoid tumors…and be a clue to diagnosis
Beta catenin is a protein found in cells throughout the body. One of the roles of beta catenin is to help regulate “cell signaling.”13 Cell signaling can instruct cells in the body when to grow and divide. Abnormal cell signaling may lead to tumor development and growth.14 Medical experts have found that beta catenin often accumulates excessively in desmoid tumors cells, causing tumors to overgrow.13
Beta catenin staining can help a pathologist determine whether a tumor is a desmoid tumor when they look at it under the microscope. Based on medical studies, 60% to 98% of desmoid tumors show beta catenin staining under a microscope.11
Knowledge is power
What questions should you ask your doctor? What are your options or next steps for desmoid tumor care? These are important aspects of making informed decisions for your health. These guides can help:
Lipoma is a common misdiagnosis for those with desmoid tumors6,†
What are lipomas?
Lipomas are abnormal, benign growths of fatty tissue. Like desmoid tumors, they can appear anywhere in the body.15,16
Lipomas are the most common type of soft tissue tumor.15 They occur far more frequently than desmoid tumors.15
- 50% of soft-tissue tumors are lipomas17
- 3% of soft-tissue tumors are desmoid tumors16
The rarity of desmoid tumors compared to lipomas may be one reason that desmoid tumors could be misdiagnosed as lipomas.5 For instance, among a sample of people whose desmoid tumors were initially misdiagnosed, 4 out of 10 tumors were mistaken for lipomas.6,*
From market research conducted by SpringWorks Therapeutics.6
Desmoid tumors and their “tendril-like” growths may be difficult to see fully using imaging tests like MRI, CT scans, or ultrasound.18 This may be another reason that a desmoid tumor could be misdiagnosed as a lipoma or another tumor type. Under a microscope, the cells of a lipoma look very different than the cells of a desmoid tumor.11,15 A biopsy of the tumor is the only way to see these differences before surgery. Ask your doctor whether a biopsy is appropriate for you.
What are some important differences between lipomas and desmoid tumors?
- Age of patients affected: while desmoid tumors are diagnosed most frequently in younger adults (age 20-44), lipomas are more common in adults aged 40-6015,19
- Considerations for surgery: The infiltrative nature of desmoid tumors may make them challenging to remove surgically. Their “tendril-like” growths can extend into layers of tissue beyond the tumor itself.5 In contrast, lipomas are generally well-defined within a thin capsule of tissue.19 After surgery, lipomas generally do not recur (come back).15
- Desmoid tumors, however, can come back after surgery. It is reported that desmoid tumors may come back 24% to 77% of the time.21,22 The risk of having desmoid tumors come back after surgery can be higher for younger patients and those with larger tumors. Tumor location is also important. Desmoid tumors in the extremities (arms, legs, hands, feet), chest wall, and within the abdominal cavity have a higher risk of coming back after being removed by surgery23
Questions to ask your doctor if you’ve been diagnosed with lipoma…and before treatment Read more
- What kinds of tests (imaging, biopsy, genetic testing) have been used to confirm the diagnosis? Are there any other tests available for me?
- Are there any other possible diagnoses?
- If your doctor is managing with a “watch and wait” approach, ask: When and how should the lipoma be monitored?
- If you are considering surgery, ask: What are the possible benefits and risks of surgery? Will the tumor be tested by a pathologist after surgery?
If you have questions about the diagnosis or treatment, it may be worthwhile to consult with a sarcoma specialist. You can find a sarcoma center here.‡
SpringWorks Therapeutics, Inc. is providing this link to help patients find a sarcoma specialist by region, but SpringWorks had no role in developing this list and inclusion on this list does not represent an endorsement or a recommendation from SpringWorks for any center or physician.
- Cancer.Net. Desmoid tumor: risk factors. Accessed April 8, 2024. https://www.cancer.net/cancer-types/desmoid-tumor/risk-factors
- Husson O, Younger E, Dunlop A, et al. Desmoid fibromatosis through the patients’ eyes: time to change the focus and organisation of care? Support Care Cancer. 2019;27(3):965-980.
- Hanna D, Magarakis M, Twaddell W, Alexander R, Kesmodel S. Rapid progression of a pregnancy-associated intra-abdominal desmoid tumor in post-partum period: A case report. International Journal of Surgery Case Reports. 2016 Oct;26.
- Cancer.Net. Desmoid tumor: diagnosis. Accessed April 8, 2024. https://www.cancer.net/cancer-types/desmoid-tumor/diagnosis
- Kasper B, Baumgarten C, Garcia J, et al; Desmoid Working Group. An update on the management of sporadic desmoid-type fibromatosis: a European Consensus Initiative between Sarcoma PAtients EuroNet (SPAEN) and European Organization for Research and Treatment of Cancer (EORTC)/Soft Tissue and Bone Sarcoma Group (STBSG). Ann Oncol. 2017;28(10):2399-2408.
- Data on file. SpringWorks Therapeutics.
- Penel N, Coindre JM, Bonvalot S, et al. Management of desmoid tumors: a nationwide survey of labelled reference centre networks in France. Eur J Cancer. 2016;58:90-96.
- SARC (Sarcoma Alliance for Research through Collaboration). About SARC. Accessed February 15, 2024. https://sarctrials.org/about-sarc
- Referenced with permission from the NCCN Guidelines for Patients® for Soft Tissue Sarcoma, 2023. © National Comprehensive Cancer Network, Inc. 2023. All rights reserved. Accessed April 8, 2024. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use, or application, and disclaims any responsibility for their application or use in any way.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Soft Tissue Sarcoma V.1.2024. © National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed May 1, 2024. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
- Gronchi A, et al. Desmoid Tumor Working Group. The management of desmoid tumours: a joint global consensus-based guideline approach for adult and paediatric patients [supplementary appendix]. Eur J Cancer. 2020;127:96-107.
- Braschi-Amirfarzan M, Keraliya AR, Krajewski KM, et al. Role of imaging in management of desmoid-type fibromatosis: a primer for radiologists. Radiographics. 2016;36(3):767-782.
- Penel N, Chibon F, Salas S. Adult desmoid tumors: biology, management and ongoing trials. Curr Opin Oncol. 2017;29(4):268-274.
- NIH. National Cancer Institute. NCI dictionary of cancer terms: desmoid tumor. Accessed April 8, 2024. https://www.cancer.gov/publications/dictionaries/cancer-terms/expand/D
- Kolb L, Yarrarapu SNS, Ameer MA, et al. Lipoma. [Updated 2022 Jul 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507906/
- Constantinidou A, Scurr M, Judson I, Litchman C. Clinical presentation of desmoid tumors. In: Litchman C, ed. Desmoid Tumors. Springer; 2012:chap 2. Accessed February 15, 2024. https://www.researchgate.net/publication/226455135
- Li M, Zhang L, Xu XJ, Shi Z, Zhao XM. CT and MRI features of tumors and tumor-like lesions in the abdominal wall. Quant Imaging Med Surg. 2019;9(11):1820-1839.
- Rosa F, Marinetti C, Piscopo F, et al. Multimodality imaging features of desmoid tumor: a head-to-toe spectrum. Insights into Imaging. 2020;11(1):1-3.
- van Broekhoven DLM, Grünhagen DJ, den Bakker MA, van Dalen T, Verhoef C. Time trends in the incidence and treatment of extra-abdominal and abdominal aggressive fibromatosis: a population-based study. Ann Surg Oncol. 2015;22(9):2817-2823.
- Charifa A, Azmat CE, Badri T. Lipoma Pathology. [Updated 2021 Dec 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482343/
- Easter DW, Halasz NA. Recent trends in the management of desmoid tumors. Summary of 19 cases and review of the literature. Ann Surg. 1989;210(6):765-769.
- Skubitz KM. Biology and treatment of aggressive fibromatosis or desmoid tumor. Mayo Clin Proc. 2017;92(6):947-964.
- Crago AM, Denton B, Salas S, et al. A prognostic nomogram for prediction of recurrence in desmoid fibromatosis. Ann Surg. 2013;258(2):347-353.



