Approximately 30% to 40% of desmoid tumors are initially misdiagnosed due to their rarity and histologic mimics.1
Common misdiagnoses include:2-4,*
- Hypertrophic or procedure-related scars
- Keloid scars
- Nodular fasciitis
- Fibromas
- Lipomas
- Low-grade sarcomas
- Gastrointestinal stromal tumor (GIST)
- Nerve sheath tumor (schwannoma)
- Smooth muscle tumor (leiomyoma)
Data derived from an online survey of 130 oncologists and surgeons who treat desmoid tumors, conducted by SpringWorks Therapeutics between February and March 2022. Responses were collected from a comprehensive review of 361 desmoid tumor patient charts. Physicians (n=30) were asked to consider the primary diagnosis their patients with desmoid tumors initially received.2
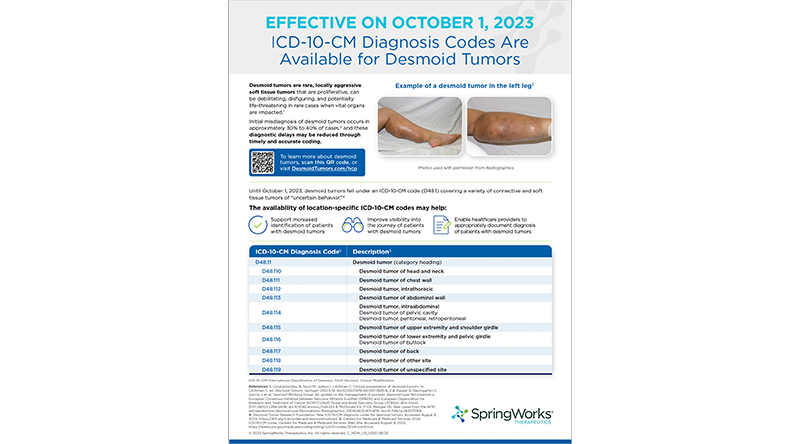
ICD-10-CM codes for desmoid tumors
Location-specific ICD-10-CM codes for desmoid tumors went into effect on October 1, 2023.5 The codes help enable healthcare providers to appropriately document diagnoses of patients with desmoid tumors and may help improve patient care.
| ICD-10-CM Diagnosis Code5 | Description5 |
|---|---|
| D48.11 | Desmoid tumor (category heading) |
| D48.110 | Desmoid tumor of head and neck |
| D48.111 See all |
Desmoid tumor of chest wall |
| D48.112 | Desmoid tumor, intrathoracic |
| D48.113 | Desmoid tumor of abdominal wall |
| D48.114 | Desmoid tumor, intraabdominal Desmoid tumor of pelvic cavity Desmoid tumor, peritoneal, retroperitoneal |
| D48.115 | Desmoid tumor of upper extremity and shoulder girdle |
| D48.116 | Desmoid tumor of lower extremity and pelvic girdle Desmoid tumor of buttock |
| D48.117 | Desmoid tumor of back |
| D48.118 | Desmoid tumor of other site |
| D48.119 | Desmoid tumor of unspecified site |
Location-specific ICD-10-CM diagnosis codes for desmoid tumors can be incorporated into your clinical practice.
Guidelines Recommend Consulting With Desmoid Tumor Experts
The NCCN Guidelines† and Desmoid Tumor Working Group (DTWG)‡ Guideline recommend an initial evaluation and management by a multidisciplinary team with expertise and experience in desmoid tumors.6,7 Collaborating with specialists may improve prognoses and patients’ quality of life.8,9
The National Comprehensive Cancer Network® (NCCN®) is a not-for-profit alliance of 33 leading cancer centers devoted to patient care, research, and education. The development of the NCCN Guidelines is an ongoing and iterative process based on a critical review of the best available evidence and derivation of recommendations by a multidisciplinary panel of experts in the field of cancer.6
The Desmoid Tumor Working Group (DTWG) consists of more than 90 sarcoma experts, patients, and patient advocates from around the world. The DTWG includes representatives from all disciplines involved in the management of desmoid tumors, including pathology, molecular biology, radiology, orthopedic surgery, surgical oncology, radiotherapy, medical oncology, and supportive care.7
Leveraging Diagnostic Tools for Timely and Accurate Diagnosis
Initial clinical evaluation pre-diagnosis
- Ultrasound is an affordable option for initial imaging of small, palpable, benign-looking lesions to estimate size and relation to fascia10
- Ultrasound may be implemented as the initial imaging approach, but it should be followed by CT or MRI10
- High risk features for soft tissue tumors that should prompt further workup:10
- Recent increase in size
- Deep location relative to fascia
Diagnostic Tools

Imaging
NCCN Guidelines recommend the following prior to initiation of a treatment plan for progressive, morbid, or symptomatic disease:6
- CT/MRI scan
- Core biopsy

Core Needle Biopsy and Nuclear Beta-Catenin Staining
Histopathologic assessment and immunostaining for beta-catenin are important for diagnosis of desmoid tumors.11 The DTWG Guideline identifies nuclear positivity for beta-catenin as the key immunophenotypic feature of desmoid tumors.12 See staining
The presence of nuclear immunopositivity for beta-catenin has been reported in 80% to 98% of sporadic desmoid tumor cases and 60% to 70% of FAP-associated desmoid tumor cases.12

Genetic Testing
The DTWG Guideline recommends:
- Performing a mutational analysis in desmoid tumor biopsy specimens to confirm diagnosis and guide the workup when appropriate. The use of a next-generation sequencing (NGS)-based diagnostic approach appears to be more sensitive12
- 85% to 90% of desmoid tumors are sporadic and most often associated with activating mutations of the beta-catenin gene CTNNB112,13
- 10% to 15% of desmoid tumors are syndromic in the context of familial adenomatous polyposis (FAP) and associated with germline inactivating mutations in APC 12,13
Radiology & Pathology of Desmoid Tumors
Approximately 30%-40% of desmoid tumors are initially misdiagnosed.1
Learn more about tools and tests to help provide a timely, accurate diagnosis for your patients.

Imaging
Despite being infiltrative, many desmoid tumors may appear well-circumscribed, or entrapped and atrophied muscle may be mistaken for malignancy.14
CT is preferable for intra-abdominal desmoid tumors and associated complications14

Contrast-enhanced CT showed a large unresectable mesenteric desmoid tumor (arrowheads) closely associated with mesenteric vessels (arrow)15
The tumor was originally identified during pregnancy and suspected to be an ovarian mass prior to biopsy15
MRI can provide clues to histology and progression risk14,16
Hyperintense T2 signal is associated with high cellularity and increased risk of desmoid tumor progression14,16

T2-weighted MRI scan showed hyperintensity and ill-defined margins (white arrows) of a progressing axilla desmoid tumor17
This tumor was initially misdiagnosed as a sarcoma on preoperative CT but correctly diagnosed by MRI17

Core Needle Biopsy and Nuclear Beta-Catenin Staining
The heterogeneous morphology of desmoid tumors can make diagnosis challenging18
- On average, desmoid tumors have 2 distinct histologic patterns, but some may demonstrate up to 5 patterns, with intra-abdominal tumors having the greatest variability18
- The 3 most common histologic patterns, any of which may be observed in a single tumor, are shown below:18

Conventional
100% of cases—sweeping fascicles of uniform spindle fibroblasts with little cell-to-cell contact, abundant collagen and blood vessels18
Mitoses and atypia are rarely seen18,19

Hypocellular/hyalinized
28% of cases—decreased cellular density and increased stromal hyalinization18
Although fibroblasts are still present, they are typically widely spaced and set in a densely eosinophilic matrix18

Staghorn Vessel
21% of cases—thin-walled branched blood vessels lined by a single layer of flat to ovoid endothelial cells that appear hyperchromatic relative to the lighter staining stromal cells18
In addition to heterogeneous morphology, accurate diagnosis is also complicated due to histologic mimics1
Low-grade sarcomas, GIST, nodular fasciitis, and other histologic mimics can often be differentiated from desmoid tumors through a combination of histologic findings and ancillary testing, with examples below:4,18,20

Low-grade fibromyxoid sarcoma with focal nuclear atypia that is rare in desmoid tumors18,21
Absence of nuclear beta-catenin staining and positivity for MUC4 by immunohistochemistry, and FUS gene rearrangements, can help distinguish low-grade fibromyxoid sarcomas from desmoid tumors18,22

Desmoid tumor with characteristic nuclear beta-catenin staining1
Presence of CTNNB1 or APC mutations can help confirm a desmoid tumor diagnosis4,18

June 24, 2024.
GIST with diffuse DOG1 staining that is not observed in desmoid tumors23,24
Absence of nuclear beta-catenin and positivity for CD117 (c-kit) can help distinguish GIST from desmoid tumors4,18
Detection of certain gene fusions using molecular techniques

Nodular fasciitis with USP6 gene rearrangement by FISH (separation of red and green dots)25
A high mitotic index and absence of nuclear beta-catenin can help distinguish nodular fasciitis from desmoid tumors18,20,22
CT, computed tomography; FISH, fluorescence in situ hybridization; GIST, gastrointestinal stromal tumor; ICD-10-CM, International Classification of Diseases, Tenth Revision, Clinical Modification; IV, intravenous; MRI, magnetic resonance imaging; NCCN, National Comprehensive Cancer Network® (NCCN®).
- Kasper B, Baumgarten C, Garcia J, et al. Desmoid Working Group. An update on the management of sporadic desmoid-type fibromatosis: a European Consensus Initiative between Sarcoma PAtients EuroNet (SPAEN) and European Organization for Research and Treatment of Cancer (EORTC)/Soft Tissue and Bone Sarcoma Group (STBSG). Ann Oncol. 2017;28(10):2399-2408.
- Data on file: SpringWorks Therapeutics.
- Penel N, Coindre JM, Bonvalot S, et al. Management of desmoid tumours: a nationwide survey of labelled reference centre networks in France. Eur J Cancer. 2016;58:90-96.
- Huss S, Nehles J, Binot E, et al. β-catenin (CTNNB1) mutations and clinicopathological features of mesenteric desmoid-type fibromatosis. Histopathology. 2013;62(2):294-304.
- Centers for Medicare & Medicaid Services 2024 ICD-10-CM codes. Centers for Medicare & Medicaid Services Web Site. Accessed July 26, 2024. https://www.cms.gov/medicare/coding-billing/icd-10-codes/2024-icd-10-cm.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Soft Tissue Sarcoma V.2.2024. © National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed August 9, 2024. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
- Kasper B, Baldini EH, Bonvalot S, et al; Desmoid Tumor Working Group. Current management of desmoid tumors: a review. JAMA Oncol. Accessed July 26, 2024. https://jamanetwork.com/journals/jamaoncology/article-abstract/2820212.
- Husson O, Younger E, Dunlop A, et al. Desmoid fibromatosis through the patients’ eyes: time to change the focus and organisation of care? Support Care Cancer. 2019;27(3):965-980.
- Joglekar SB, Rose PS, Sim F, Okuno S, Petersen I. Current perspectives on desmoid tumors: the Mayo Clinic approach. Cancers (Basel). 2011;3(3):3143-3155.
- Smolle MA, Andreou D, Tunn PU, et al. Diagnosis and treatment of soft-tissue sarcomas of the extremities and trunk. EFORT Open Rev. 2017;2(10):421-431.
- Carlson JW, Fletcher CDM. Immunohistochemistry for β-catenin in the differential diagnosis of spindle cell lesions: analysis of a series and review of the literature. Histopathology. 2007;51(4):509-514.
- Kasper B, Baldini EH, Bonvalot S, et al; Desmoid Tumor Working Group. Current management of desmoid tumors: a review [supplementary online content]. JAMA Oncol. Accessed July 26, 2024. https://jamanetwork.com/journals/jamaoncology/article-abstract/2820212.
- Penel N, Chibon F, Salas S. Adult desmoid tumors: biology, management and ongoing trials. Curr Opin Oncol. 2017;29(4):268-274.
- Rosa F, Martinetti C, Piscopo F, et al. Multimodality imaging features of desmoid tumors: a head-to-toe spectrum. Insights Imaging. 2020;11(1):103
- Shinagare AB, Ramaiya NH, Jagannathan JP, et al. A to Z of desmoid tumors. AJR Am J Roentgenol. 2011;197(6):W1008-W1014.
- Cassidy MR, Lefkowitz RA, Long N, et al. Association of MRI T2 signal intensity with desmoid tumor progression during active observation: a retrospective cohort study. Ann Surg. 2020;271(4):748-755.
- Xu H, Koo HJ, Lim S, et al. Desmoid-type fibromatosis of the thorax: CT, MRI, and FDG PET characteristics in a large series from a tertiary referral center. Medicine (Baltimore). 2015;94(38):e1547.
- Zreik RT, Fritchie KJ. Morphologic spectrum of desmoid-type fibromatosis. Am J Clin Pathol. 2016;145(3):332-340.
- Soft Tissues: Desmoid-type fibromatosis. Atlas of Genetics and Cytogenetics in Oncology and Haematology website. Written 2013. Accessed July 26, 2024. https://atlasgeneticsoncology.org/solid-tumor/5179/soft-tissues-desmoid-type-fibromatosis.
- Sbaraglia M, Bellan E, Dei Tos AP. The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives. Pathologica. 2021;113(2):70-84.
- Li M, Chen H, Shi D, Chen M, Zhang Z, Zhang H. Low-grade fibromyxoid sarcoma: a clinicopathologic and molecular study of 10 genetically confirmed cases. Int J Clin Exp Pathol. 2018;11(12):5860-5868.
- Bhattacharya B, Dilworth HP, Iacobuzio-Donahue C, et al. Nuclear beta-catenin expression distinguishes deep fibromatosis from other benign and malignant fibroblastic and myofibroblastic lesions. Am J Surg Pathol. 2005;29(5):653-659.
- Liang T, Chopra S. GIST. PathologyOutlines.com website. Accessed July 26, 2024. https://www.pathologyoutlines.com/topic/smallbowelGIST.html.
- West RB, Corless CL, Chen X, et al. The novel marker, DOG1, is expressed ubiquitously in gastrointestinal stromal tumors irrespective of KIT or PDGFRA mutation status. Am J Pathol. 2004;165(1):107-113.
- Emori M, Shimizu J, Murahashi Y, et al. Nodular fasciitis involving the palm. Ann R Coll Surg Engl. 2018;100(5):e128-e131.



